In this article, you’ll learn about the role of cannabis in palliative care. Insight Archives provides information and analysis on the cannabis industry in Canada, covering various topics such as pricing trends, distribution models, quality assurance standards, and provincial regulations. We discuss recent issues like the misreporting of cannabis edibles and distribution models in Saskatchewan and Manitoba, as well as the challenges faced by local cannabis producers. We also explore emerging trends like the use of cannabis for women’s health and the growth of cannabis consumption lounges.
Understanding the Role of Cannabis in Palliative Care
This image is property of media.capc.org.
Introduction
Palliative care plays a crucial role in providing comfort and support to patients with life-limiting illnesses. It focuses on improving the quality of life for individuals and their families by addressing physical, emotional, and spiritual needs. This article aims to explore the potential benefits and challenges of integrating cannabis into palliative care and its impact on patient well-being.
Exploring the Concept of Palliative Care
Palliative care is a specialized medical approach that provides compassionate care to patients with life-limiting illnesses. It focuses on alleviating pain and symptoms, as well as offering emotional and spiritual support to patients and their families. Palliative care aims to improve the overall quality of life for individuals facing serious illnesses, regardless of their age or prognosis.
The Role of Palliative Care in Providing Comfort and Support
Palliative care professionals work collaboratively with patients, families, and other healthcare providers to address the physical, emotional, and spiritual needs of individuals with life-limiting illnesses. They can help manage symptoms such as pain, nausea, and insomnia, and provide holistic support to enhance overall well-being.
Addressing the Needs of Patients with Life-Limiting Illnesses
Patients with life-limiting illnesses often face various physical, emotional, and psychological challenges. Palliative care professionals aim to address these needs by providing appropriate symptom management, counseling, and support. The focus is on enhancing the patient’s quality of life and respecting their autonomy and choices.
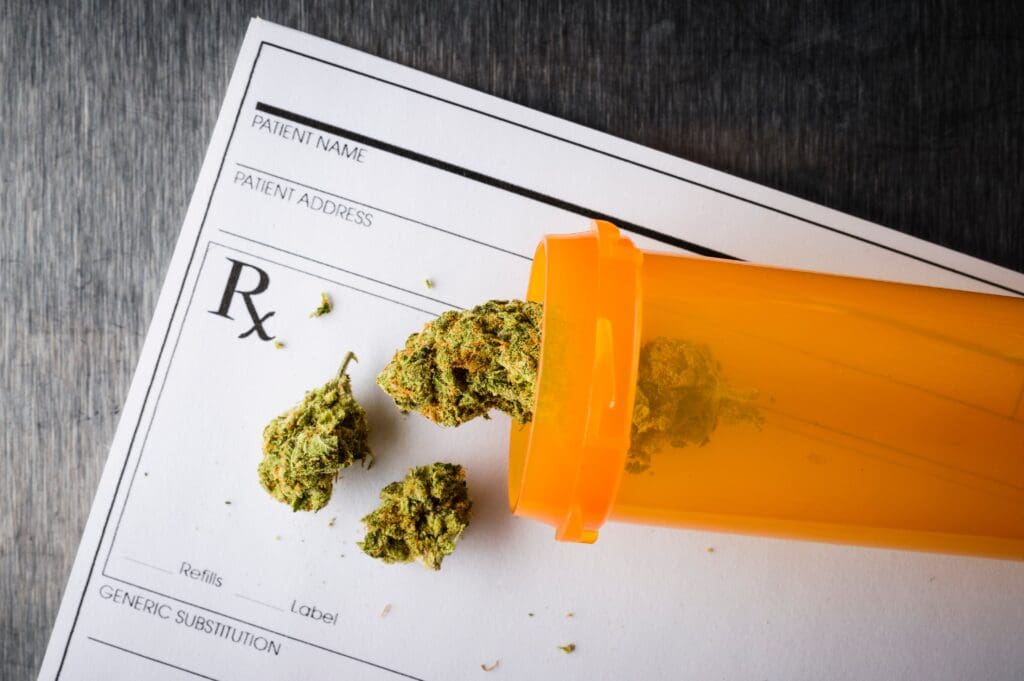
This image is property of www.mdpi.com.
Overview of Cannabis and Its Components
Cannabis, also known as marijuana, is a plant with various active components, including cannabinoids. The two primary cannabinoids are tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is responsible for the psychoactive effects of cannabis, while CBD is non-intoxicating and has potential therapeutic benefits.
Different Types of Cannabis Products
Cannabis is available in various forms, including dried flowers, oils, tinctures, topicals, edibles, and capsules. Each product has different effects and methods of administration. Understanding the different types of cannabis products is essential for healthcare professionals and patients when considering its use in palliative care.
Legality and Regulatory Framework Surrounding Cannabis
The legal status of cannabis varies across different jurisdictions. In Canada, cannabis for medical purposes is legal, regulated, and accessible through authorized producers. It is important for healthcare professionals to be aware of the legal and regulatory framework surrounding cannabis to ensure compliance and patient safety.
Understanding the Potential Therapeutic Effects of Cannabis
Cannabis has been shown to have potential therapeutic effects, particularly in managing pain, nausea, and appetite stimulation. It can also help alleviate symptoms such as anxiety, depression, and insomnia. These potential benefits make cannabis an intriguing option for integration into palliative care.
Managing Pain and Symptoms with Cannabis
Pain management is a significant aspect of palliative care, and cannabis can play a role in alleviating pain symptoms. The cannabinoids in cannabis have been found to have analgesic properties, potentially providing relief to patients experiencing pain associated with their illness. However, it is crucial to assess individual patient needs and preferences to determine the most suitable treatment approach.
Improving Quality of Life for Palliative Care Patients
The integration of cannabis into palliative care can significantly improve the quality of life for patients. Cannabis can enhance appetite, relieve nausea, promote relaxation, and reduce anxiety and depression. These benefits can contribute to a better overall quality of life for individuals facing life-limiting illnesses.
Cautions and Side Effects of Cannabis Use
While cannabis can offer potential benefits, it is essential to be aware of potential cautions and side effects. Cannabis use can lead to short-term effects such as dizziness, dry mouth, and impaired cognitive function. It may also have interactions with other medications or have varying effects on individuals with specific medical conditions. Healthcare professionals must carefully assess the risks and benefits of cannabis use in each patient.
Assessing Individual Patient Needs and Preferences
When considering cannabis as a treatment option in palliative care, healthcare professionals must assess each patient’s individual needs, preferences, and goals. This assessment includes evaluating their medical condition, past experiences with cannabis (if any), and any potential contraindications or drug interactions. Taking a comprehensive approach ensures that cannabis use aligns with the patient’s overall care plan.

This image is property of d2jx2rerrg6sh3.cloudfront.net.
Drug Interactions and Contraindications with Cannabis
Cannabis can interact with certain medications, both prescription and over-the-counter. Healthcare professionals must consider potential drug interactions and contraindications before recommending cannabis use. It is crucial to educate patients about the importance of disclosing their medication history to ensure safe and effective cannabis integration.
Methods of Administration for Cannabis in Palliative Care
Cannabis can be administered in various ways to accommodate individual preferences and needs. Smoking and vaporizing are common methods, offering fast-acting relief. Ingesting cannabis edibles provides a longer-lasting effect. Topical applications and oils can be used for localized pain relief. Each method has different effects and considerations, and healthcare professionals should guide patients in choosing the most appropriate method.
Determining Appropriate Dosage Levels
Finding the right dosage of cannabis is essential to ensure optimal therapeutic effects while minimizing side effects. Healthcare professionals need to consider factors such as the patient’s tolerance, desired outcomes, and potential drug interactions when determining appropriate dosage levels. Starting with a lower dose and gradually increasing it allows for individualized care and monitoring.
Monitoring the Effects of Cannabis on Patients
Regular monitoring of patients’ response to cannabis is crucial in palliative care. Healthcare professionals should assess the effectiveness of cannabis in managing symptoms, as well as any side effects experienced. Patient feedback and open communication are valuable in determining the appropriateness of cannabis use and making necessary adjustments to dosage or administration method.

This image is property of 149884669.v2.pressablecdn.com.
Adjusting Dosage Based on Individual Responses
As with any medication, individual responses to cannabis can vary. Healthcare professionals must be flexible in adjusting the dosage based on the patient’s response and feedback. Regular monitoring ensures that patients receive optimal therapeutic benefits while minimizing potential side effects.
Navigating Legal Frameworks and Regulations
When integrating cannabis into palliative care, healthcare professionals must navigate legal frameworks and regulations. Staying informed about current legislation and adhering to regulatory requirements ensures compliance and patient safety. Collaboration with legal professionals can provide guidance on the legal aspects of cannabis use in palliative care settings.
Ethical Considerations of Cannabis Use in Healthcare
The use of cannabis in healthcare raises ethical considerations that healthcare professionals must address. Ethical principles such as patient autonomy, beneficence, and non-maleficence should guide decision-making. Respecting patients’ preferences, providing accurate information, and involving them in the decision-making process are essential in ensuring ethical cannabis use in palliative care.
Patient Autonomy and Informed Consent
Respecting patient autonomy is paramount in healthcare decision-making. In the context of cannabis use in palliative care, healthcare professionals should provide comprehensive information about the potential benefits, risks, and alternatives. Obtaining informed consent ensures that patients can make informed choices aligned with their values and goals of care.
Providing Comprehensive Information about Cannabis
Education and counseling are crucial components of integrating cannabis into palliative care. Healthcare professionals play a vital role in providing comprehensive information to patients and their families about cannabis, including its potential benefits, risks, and methods of administration. Clear and accurate communication helps patients make informed decisions and have realistic expectations.
Addressing Concerns and Misconceptions
There may be concerns and misconceptions surrounding cannabis use in palliative care. Healthcare professionals should create a supportive environment to address these concerns openly. Providing evidence-based information and addressing misconceptions can help patients and their families make informed decisions about cannabis use as part of their palliative care plan.
Supporting Patients and Caregivers in Decision-Making
The decision to incorporate cannabis into palliative care is a collaborative process between patients, families, and healthcare professionals. Supportive counseling and guidance from healthcare professionals can help patients and their families navigate the complexities of cannabis use. Ensuring that patients and caregivers are well-supported throughout the decision-making process fosters a partnership approach to care.
Collaboration between Healthcare Professionals and Cannabis Experts
Integrating cannabis into palliative care requires collaboration between healthcare professionals and cannabis experts. These experts can provide specialized knowledge regarding cannabis strains, dosing, and administration, while healthcare professionals contribute their clinical expertise. By working together, they can develop comprehensive care plans that address the unique needs of each patient.
Integrating Cannabis into Existing Treatment Plans
Cannabis should be considered as part of an overall treatment plan in palliative care. By integrating cannabis with other palliative care interventions, healthcare professionals can provide a tailored approach to addressing patients’ symptoms and improving their quality of life. Regular communication and collaboration among healthcare providers ensure that patients receive comprehensive and coordinated care.
Developing Guidelines and Protocols for Cannabis Use
To ensure safe and effective cannabis use in palliative care, guidelines and protocols need to be developed. These guidelines can provide healthcare professionals with standardized approaches to prescribing, monitoring, and adjusting cannabis treatment. Collaboration with regulatory bodies, legal professionals, and industry experts helps establish best practices and ensures quality care.
Summarizing the Role of Cannabis in Palliative Care
Cannabis has the potential to play a valuable role in palliative care by providing relief from pain and symptoms, enhancing quality of life, and addressing the holistic needs of patients. Integrating cannabis into palliative care requires thorough assessment, individualized treatment plans, and ongoing monitoring. Healthcare professionals must navigate legal and ethical considerations while providing comprehensive education and support to patients and their families.
Highlighting the Potential Benefits and Challenges
The integration of cannabis into palliative care offers potential benefits for patients facing life-limiting illnesses. It can provide relief from symptoms, improve overall well-being, and enhance quality of life. However, challenges such as legal and regulatory complexities, potential side effects, and individual variations must be carefully addressed. Comprehensive education and ongoing monitoring are essential to ensure safe and effective cannabis use.
Emphasizing the Need for Further Research and Education
While cannabis shows promise in palliative care, further research and education are needed to better understand its potential benefits, risks, and interactions. Continued research can provide evidence-based guidelines, further validating the role of cannabis in palliative care. Healthcare professionals should stay updated on the latest advancements and collaborate with researchers to contribute to the growing knowledge base.
In conclusion, the integration of cannabis into palliative care holds promise for providing relief and enhancing the overall quality of life for patients with life-limiting illnesses. Healthcare professionals play a crucial role in assessing patient needs, providing education and counseling, and monitoring the effects of cannabis use. As the legal and regulatory landscape evolves, collaboration between healthcare professionals, cannabis experts, researchers, and policymakers is paramount in ensuring safe and effective cannabis integration in palliative care settings.